Shoulder Replacement Surgery FAQ
Shoulder replacement surgery is one of the most common procedures I perform. The most common reasons patients require shoulder replacement surgery is due to osteoarthritis of the shoulder, however it may also be indicated in patients with large rotator cuff tears and/or fractures of the shoulder. Below is a list of the most common questions patients ask me about shoulder replacement surgery.
Q: Will I need any tests done before I am ready for surgery?
A: After the decision has been made to proceed with shoulder replacement surgery, typically two things are required prior to your surgical date.
- A CT scan of the shoulder – I use the CT scan of the shoulder to plan each patient’s surgery to determine which shoulder replacement components will best fit an individual patient’s anatomy. Also, in many cases I use the CT scan to have custom patient specific instrumentation made to ensure that the implants are placed in an optimal position.
- Pre-operative clearance from your primary care physician to ensure that there are no medical conditions that would make undergoing shoulder replacement surgery unsafe.
Q: How long is the surgery?
A: The length of the surgery can vary significantly depending on the patient’s anatomy, but on average it takes approximately 1.5-2 hours to complete.
Q: What is the recovery like after shoulder replacement surgery?
A: Typically, patient will have to be in a sling for 4-6 weeks after the surgery. After the sling is discontinued patients can move the shoulder as they tolerate, however I will ask patients to limit heavy lifting until ~10-12 weeks after the surgery. Patients should begin physical therapy 2-4 weeks after surgery and will continue until about 3-4 months after the surgery.
Q: What are the benefits of shoulder replacement surgery?
A: Most patients will experience resolution of most of their pain with activities of daily living. Most patients will experience significant improvements in their range of motion after surgery as well. Depending on patients’ pre-operative limitations, patients are often able to perform activities that they were unable to perform prior to the surgery.
Q: Will I have to stay in hospital over night after my shoulder replacement surgery?
A: Most patients I treat with shoulder replacements go home only a couple hours after the surgery is complete. In some cases, depending on a patient’s medical history and functional status, I may ask them to stay in hospital overnight for observation.
Q: What is the difference between an anatomic total shoulder replacement and a reverse total shoulder replacement?
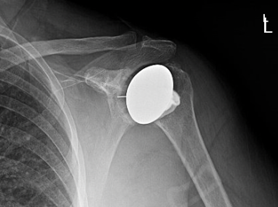
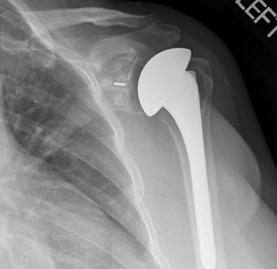
A: The shoulder is a ball and socket joint, with the glenoid forming the socket and the humeral head making up the ball portion of the joint. In an anatomic shoulder replacement the humeral head is replaced with a new ball shaped prosthesis and a new prosthetic cup is placed where the glenoid was previously located. In a reverse total shoulder replacement, the anatomy is flipped, and the prosthetic cup is placed where the humeral head was, and the new ball of the shoulder is placed on the glenoid. A reverse total shoulder arthroplasty is more ideal in patients with issues with their rotator cuff as the change in anatomy allows for the deltoid to perform many of the functions of the rotator cuff.


Q: How do I know when I am “ready” for shoulder replacement surgery
A: The timing of shoulder replacement varies depending on the individual patient. Generally once patients reach the point that they feel their shoulder is affecting their everyday life, despite having tried non-operative treatment options such as therapy, anti-inflammatory medications, and cortisone injections. Patients who choose to undergo shoulder replacement surgery often will state that they must restrict some activities that they do as a result of their shoulder and/or that their shoulder affects their sleep.
Q: What are the risks associated with shoulder replacement surgery?
A: Overall shoulder replacement surgery is safe with low risks of complications for most patients. However, with any surgical procedures there are risks. Risks include (but are not limited to) risk of fracture of the bone, dislocation of the prosthesis, persistent pain, stiffness, infection, wound complications, medical complications, risks of anesthetic, as well as others.
Q: What type of anesthetic is used?
A: The majority of shoulder replacements I do are done with both a general anesthetic and a nerve block. The general anesthetic means that you will be completely asleep during the procedure and that you will not remember any parts of the operation. The nerve block means that your arm will be numb for approximately 24 hours after the operation. This is highly effective at controlling pain during the first day after the surgery, which is typically the most painful portion of the procedure.
Q: Am I too young for shoulder replacement surgery?
A: There is no specific age cut-off for shoulder replacement surgery. The decision to proceed with shoulder replacement surgery in younger patients is based off several factors including the age of the patient, the severity of symptoms and the appropriateness of alternative treatment options. More modern shoulder replacement implants that I use in my practice are bone preserving and therefore more suitable for younger patients who many require a revision in their lifetime, as more of the native bone stock is maintained in the initial operation.
Dr. Nolan Horner is an orthopedic surgeon with a specialization in sports and shoulder surgery. He works in the Chicagoland area and has offices in Chicago, Oak Park, Oak Brook and St. Charles.
