ACL reconstruction surgery is one of the most common procedures I perform. The primary reason patients require ACL reconstruction surgery is due to a near complete or complete tear of the ACL. Below is a list of the most common questions patients ask me about ACL reconstruction surgery.
Q: What is the ACL, and what does it do?
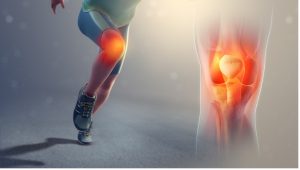
A: The Anterior Cruciate Ligament (ACL) is a cable-like structure that attaches the thigh bone (femur) to the shin bone (tibia) through the middle of the knee joint. The ACL stabilizes the knee joint by preventing the tibia from moving too far forward with respect to the femur as well as providing rotational support to the knee.
Q: Will I need any tests done before I am ready for surgery?
A: An MRI will be necessary prior to surgery to confirm the diagnosis and look for the existence of other simultaneous injuries to the knee, such as meniscal tears. After the decision has been made to proceed with ACL Reconstruction surgery, the patient may require pre-operative clearance from a primary care physician to ensure that there are no underlying medical conditions that would make undergoing ACL reconstruction surgery unsafe.
Q: How long is the surgery?
A: The length of the surgery can vary depending on the level of damage within the knee, but on average it takes approximately 1 hour to complete.
Q: What is the difference between ACL reconstruction with and without meniscus repair?
A: Injuries to the ACL are often associated with tears in the meniscus, the cartilage cushion between the femur and tibia. During ACL reconstruction surgery, if the meniscus is torn, I will either repair or remove the damaged meniscus tissue. The decision of repair versus removal is determined based on the location and severity of the tear. If the meniscus is able to be repaired, the patient will have a longer non-weightbearing period immediately after surgery to allow the meniscus to heal. The detailed rehab protocol for each operation can be found on the rehabilitation section of this website.
Q: What is the recovery like after ACL reconstruction surgery?
A: The initial recovery after an ACL reconstruction surgery varies depending on the patient’s associated meniscus procedure. If the meniscus is repaired, the patient will be restricted to toe touch weightbearing only for 2-6 weeks with no range of motion past 90 degrees for the first 4 weeks. Crutches will be necessary until 6 weeks after ACL reconstruction with meniscus repair. If there is no meniscus injury or the damaged meniscus tissue is removed, the patient can begin weightbearing and range of motion exercises up to 90 degrees as tolerated immediately after surgery. Crutches may be used as needed for the first 2 weeks after ACL reconstruction without meniscus repair.
Physical therapy for progressive strengthening and range of motion will be an essential part of ACL reconstruction recovery and should start as soon as possible after surgery. Regardless of the accompanying meniscus procedure, the earliest a patient may begin running after ACL reconstruction surgery is 3.5 months, and the earliest they may return to sports is 6 months. The detailed rehabilitation protocol for ACL reconstruction can be found on the rehabilitation section of the website.
Q: What are the benefits of ACL reconstruction surgery?
A: The ACL is necessary to provide stability during jumping, cutting, and pivoting. Once the knee has recovered from surgery, patients will experience a return to pre-injury levels of stability during these movements. The stability in the knee provided by ACL reconstruction also helps to prevent further injury to other knee structures and may to delay the onset of osteoarthritis.

Q: Will I have to stay in hospital over night after my ACL reconstruction surgery?
A: Most patients I treat with ACL reconstructions go home within a couple hours after the surgery is complete. In some rare cases, depending on a patient’s medical history and functional status, I may ask them to stay in hospital overnight for observation.
Q: What kinds of grafts can be used in ACL reconstruction surgery?
A: There are two categories of grafts that I use in ACL reconstruction surgery: Autografts and Allografts. Autograft tissue is harvested from another part of the patient’s own body, and allograft tissue is harvested from a donor. In either category, the most common graft I use in ACL reconstruction surgery is the patellar tendon, though I may use other grafts depending on the patient’s unique circumstances. Generally, younger or more active patients will receive autografts while older or less active patients will receive allografts.
Q: How do I know if I need ACL Reconstruction Surgery?
A: The necessity of ACL reconstruction surgery varies depending on the individual patient. Generally, ACL reconstruction surgery is recommended for all younger patients, especially if they are physically active. ACL reconstruction surgery in older patients is generally recommended if they wish to return to a high level of physical activity, everyday activities are impacted by the injury, or if there are other associated injuries in the knee.
Q: What are the risks associated with ACL Reconstruction surgery?
A: Overall ACL reconstruction surgery is safe with low risks of complications for most patients. However, with any surgical procedures there are risks. Risks include (but are not limited to) risk of graft failure after returning to sport, tendinitis, persistent pain, stiffness, infection, wound complications, medical complications, risks of anesthetic, as well as others.
Q: What type of anesthetic is used?
A: All of the ACL reconstruction surgeries I do are typically done with both a general anesthetic and regional nerve block. The general anesthetic means that you will be completely asleep during the procedure and that you will not remember any parts of the operation. The regional nerve block helps to reduce pain during the initial 24 hours after the operation. This is highly effective at controlling pain during the first day after the surgery, which is typically the most painful part of the procedure.
This blog post was authored by Jack Felkner BSPh and Dr. Nolan Horner MD.
Dr. Nolan Horner is an orthopedic surgeon with a specialization in sports and shoulder surgery. He works in the Chicagoland area and has offices in Chicago, Oak Park, Oak Brook and St. Charles.
